
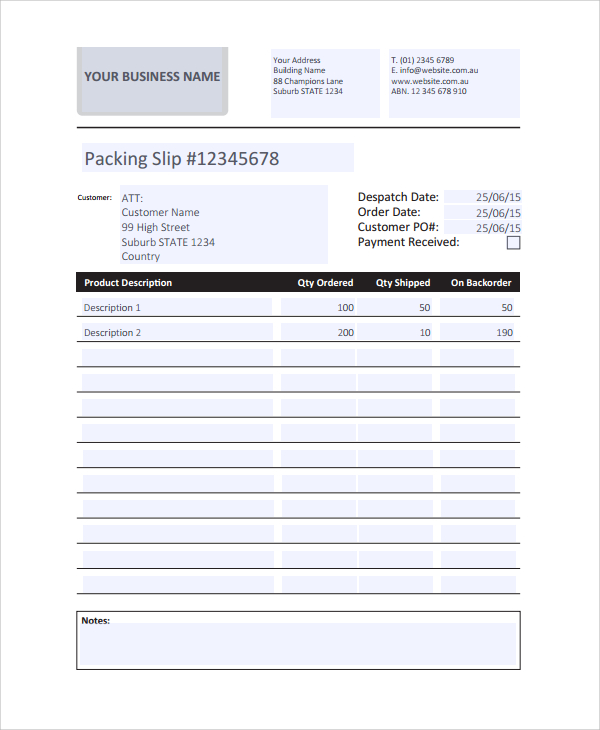
If the provider utilizes a shipping service or mail order, the proof of delivery documentation must be a complete record tracking the item(s) from the DMEPOS provider to the beneficiary. Method 2-Delivery via Shipping or Delivery Service In instances where the DMEPOS item are delivered directly by the provider, the date the beneficiary received the DMEPOS item shall be the date of service on the claim. The date of signature on the delivery slip must be the date that the DMEPOS item was received by the beneficiary or designee. *Beneficiary (or designee) signature and date of signature
#Deliveryslip add in exchange serial#
*Sufficiently detailed description of the item(s) being delivered (e.g., brand name, serial number, narrative description) If delivered to a facility, the delivery address would be the facility address *Providers are to use the address for the location where the items were delivered. The proof of delivery record must include: An example of proof of delivery to a beneficiary would be having a signed delivery slip. Providers may deliver directly to the beneficiary or the designee. Method 1-Direct Delivery to the Beneficiary By the Provider If the signature of the designee is not legible, the provider/shipping service should note the name of the designee on the delivery slip. The signature of the designee should be legible. The relationship of the designee to the beneficiary should be noted on the delivery slip obtained by the provider (i.e., spouse, neighbor, etc.). Providers, their employees, or anyone else having a financial interest in the delivery of the item are prohibited from signing and accepting an item on behalf of a beneficiary (i.e., acting as a designee on behalf of the beneficiary). “Any person who can sign and accept the delivery of durable medical equipment on behalf of the beneficiary.” Note: For the purpose of the delivery methods noted below, the designee is defined by Medicare as: Providers are required to maintain proof of delivery documentation in their files for seven years. For any services, which do not have proof of delivery from the provider, such claimed items and services shall be denied and overpayments recovered.
#Deliveryslip add in exchange mac#
Proof of delivery documentation must be made available to the DME MAC upon request. Proof of delivery is required by Medicare in order to verify that the beneficiary received the DMEPOS and is one of the provider standards as noted in 42 CFR, 424.57(12).

For more information on The MOBILITY Consultants and a menu of services we offer, visit our website at The MOBILITY Consultants. The MOBILITY Consultants is in the business of providing a comprehensive resource for mobility reimbursement and regulatory compliance issues. These added value services can help answer the questions so many suppliers have about the mobility business, increase first time approvals and assist with all audits for Medicare claims.
These added value services can help answer the questions so many suppliers have about the mobility business, increase first time approvals and assist with all audits for Medicare claims.Along with products and services to help suppliers thrive, Drive now offers information and a variety of services on Medicare reimbursement and compliance issues through The MOBILITY Consultants, LLC. Assistance in Navigating the New Medicare Market - Introducing The MOBILITY Consultants, LLCĪlong with products and services to help suppliers thrive, Drive now offers information and a variety of services on Medicare reimbursement and compliance issues through The MOBILITY Consultants, LLC.


 0 kommentar(er)
0 kommentar(er)
